Nurses Continue to Name EHRs a Top Driver of Burnout and Resignation in 2025, Black Book Nurses' Week Survey
69% Blame Poor EHR Usability for Job Dissatisfaction, 80% Consider Nurse-Friendly Systems When Job Hunting, and 2 in 3 Nurses Under 40 Say EHR Experience Impacts Employer Choice - Black Book's Sweeping 8-Month Survey Finds
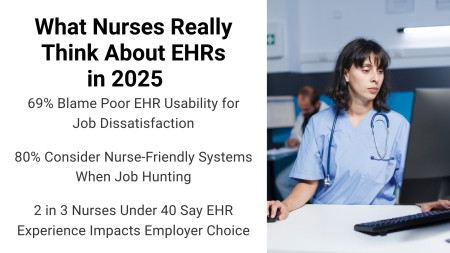
TAMPA, Fla., May 14, 2025 (Newswire.com) - A national 8-month survey conducted by Black Book Research of over 9,000 U.S. nurses - including those working in hospitals, surgery centers, physician practices, and outpatient facilities - reveals a growing disconnect between frontline nursing staff and the electronic health records (EHRs) they are expected to rely on every shift. The findings expose how poor EHR usability is not only contributing to nurse burnout but also actively driving resignations and influencing recruitment decisions.
Among the major findings:
69% of nurses say "digital documentation burden and poor EHR usability" are major contributors to their job dissatisfaction or desire to leave.
2 in 3 nurses under age 40 now rank the EHR experience among their top three factors when evaluating new employers.
80% of nurses surveyed say they would prefer to work for an employer with a "nurse-centered EHR" - a system designed with nursing input and workflow support.
"Nurses are the primary operators of healthcare technology in nearly every care setting," said Doug Brown, Founder of Black Book Research. "The EHR decisions made without the voice of nursing are the ones most likely to fail in usability, safety, and retention impact. It's time vendors and hospital IT leaders place nurses at the center of design, implementation, and optimization."
Nurse-Centered EHRs Now a Talent Magnet
The data also confirms that EHR usability has emerged as a competitive differentiator in nurse recruitment and retention. Hospitals and facilities with high nurse turnover were 3.5 times more likely to be rated by staff as using "difficult or outdated" EHRs.
In contrast, Magnet-designated hospitals which emphasize nurse leadership saw 87% of nurses rate their EHRs as "supportive to clinical workflows," compared to just 21% in non-Magnet facilities. Some health systems are already responding by including nurse satisfaction with EHRs in public-facing employer branding and onboarding campaigns.
New Nurses, Persistent Digital Barriers - and Systemic Oversights
Despite entering the workforce as digital natives, new nurses in 2025 are often blindsided by the complexity and rigidity of live EHR environments. Academic preparation frequently falls short of equipping them for the disjointed, multi-platform documentation workflows in today's hospitals and surgery centers.
In Black Book's eight-month long national survey, 88% of newly licensed nurses reported "limited or no hands-on experience" with the actual EHR systems used by their employer. Nearly all respondents (97%) agreed that nursing school courses featuring comparative overviews of major EHR platforms, workflow-specific use cases, and real-wold usability challenges would improve clinical readiness and confidence. Yet few (2%) report receiving this level of support.
Instead, nurse respondents described a troubling pattern: hospital-led EHR onboarding and optimization initiatives often driven by IT departments or outside consultants , that are overwhelmingly physician-focused. While physicians receive tailored workflows, interface customizations, and personal coaching to resolve frustrations, nurses are expected to adapt to rigid, physician-centric systems that ignore their unique workflows and daily digital burdens.
This theme carried through across all experience levels and specialties. Nurses consistently identified four major gaps where EHR vendors and system administrators are failing them:
Physician-Centric Design: Core nursing functions like bedside shift reporting, wound assessments, and medication administration are often buried deep within physician-oriented interfaces or spread across multiple disconnected tools.
Click Fatigue and Redundant Entry: Many nurses are forced to input the same patient data into three to five different systems, due to poor integration between EHRs, nurse call systems, task management apps, and documentation modules.
Lack of Mobility and Modern Input Methods: A significant 89% of nurses said they would benefit from mobile charting capabilities or voice-assisted documentation tools, especially in fast-paced environments like EDs, perioperative care, and post-op recovery.
Minimal Input and Collaboration: Only 11% of nurses surveyed believe their EHR vendor or IT department actively seeks nurse input when rolling out new features or system updates. Many felt that change decisions are made without regard for frontline clinical impact. This has not improved since an identical survey question of nurses in 2013 when 13% of nurses felt they were included in EHR development and implementation initiatives.
The resulting effect is a deepening sense of digital disempowerment, especially among younger nurses who enter the workforce eager to contribute but are quickly met with technology that inhibits efficiency, safety, and satisfaction. Until hospitals and EHR developers redefine nurses as primary users and not peripheral participants in the design and implementation process, this divide will continue to widen.," said Brown.
What Nurse-Centered EHR Design Looks Like, According to Nurses
In Black Book's 2024-2025 national survey of registered nurses, respondents outlined a consistent and practical vision for what would make EHR systems more supportive of nursing workflows. Most nurses surveyed indicated that current EHRs remain physician-centered and miss key usability features that affect bedside care.
The most commonly requested improvements from nurses across inpatient, ambulatory, and surgical settings include:
Modular Dashboards for Nursing Tasks
Customizable shift-based views that prioritize vitals, medications, alerts, and rounding needs.
Voice-Enabled Documentation
Built-in voice-to-text tools to reduce reliance on typing, particularly in high-acuity settings.
Mobile-Optimized Interfaces
Access to EHRs through phones or tablets during point-of-care tasks, especially in EDs, surgical units, and home care.
Integrated Handoff Tools
Seamless shift-change and care coordination modules that reduce duplication and errors.
Nurse Advisory Roles in EHR Development
Respondents favored formal roles for nurses in shaping new features and system upgrades.
Peer-Led EHR Training and Support
Nurses in high-satisfaction systems reported better outcomes when clinical informatics teams included experienced nurses.
Findings from Black Book's 2025 nurse survey suggest that EHR dissatisfaction among nurses is no longer a peripheral issue as it is closely tied to workforce stability, care quality, and clinician engagement. Across hospital and ambulatory settings, nurses described being left out of key performance improvement decisions that shape their daily workflows, despite being the largest and most consistent group of EHR users.
In many cases, EHR optimization and digital transformation projects led by external consultants or performance improvement teams continue to focus disproportionately on the needs of admitting and affiliated physicians. Nurses report that their input is rarely sought, and their challenges with documentation inefficiencies, workflow fragmentation, and digital redundancy are often dismissed as training issues rather than system design flaws.
This approach, according to surveyed nurses, primarily serves commercial and billing interests aligned with vendor objectives, while failing to address operational pressures that contribute to nurse attrition, burnout, and reduced time for direct patient care. In contrast to peer countries where clinician-facing digital systems have been adapted through iterative frontline feedback, U.S. hospitals risk falling behind by not treating nurse experience as a design priority.
Still, several organizations were cited by nurses in the Black Book survey as making notable and measurable progress through more inclusive digital governance:
Top 20 Nurse-Rated Health Systems for EHR Usability (2025)
As reported by registered nurses in Black Book Research's 8-month national survey for in-house initiatives focusing on Nurses' EHR Satisfaction
Health System | Notable Nurse-Centered EHR Programming |
|---|---|
Cleveland Clinic Health System (OH) | Nurse informaticists embedded in departments; point-of-care usability redesign input |
Inova Health System (VA) | Peer-led training and mentorship; nurse-specific optimization initiatives |
Cedars-Sinai Medical Center (CA) | Real-time usability tracking; nurse-run feedback and advisory groups |
Geisinger Health System (PA) | Voice-enabled documentation in nursing units; mobile-first EHR access |
Novant Health (NC) | Simulation labs for onboarding; customized EHR workflows for bedside roles |
Northwell Health (NY) | Nurse innovation lab co-develops digital tools; structured vendor collaboration |
UCHealth (CO) | Workflow analytics to streamline nursing tasks; input-driven documentation reduction |
Spectrum Health/Corewell Health (MI) | Cross-disciplinary optimization councils including bedside nurses |
Baylor Scott & White Health (TX) | Informatics bootcamps; iterative usability updates driven by nurse surveys |
University of Utah Health (UT) | Piloting voice tools for nurses; digital onboarding mentorship model |
NYU Langone Health (NY) | Nurse EHR usability liaisons across service lines; standardized rounding and handoff modules |
UCLA Health (CA) | Inclusive clinical informatics program; nurse representation in vendor R&D pilots |
Main Line Health (PA) | Nursing-led documentation redesign team; shift-based dashboard pilots |
AdventHealth (FL) | Continuous feedback loops through nursing councils; mobile tools for perioperative and med-surg units |
Rush University System for Health (IL) | Centralized nurse EHR training with clinical simulation integration |
Emory Healthcare (GA) | Post-go-live optimization clinics led by nursing teams; emphasis on charting efficiency |
Banner Health (AZ) | Real-time digital helpdesk for nursing staff; collaborative update rollout processes |
Intermountain Health (UT) | Nurse-led tech governance; system-level KPIs tracked for documentation efficiency |
Houston Methodist (TX) | EHR design informed by high-performing nurse units; rapid feedback implementation cycles |
Ochsner Health (LA) | Nurse usability taskforces; care team-centered charting modules deployed across facilities |
These top performing organizations suggest that when health systems structure technology programs around the realities of nursing practice, the benefits extend beyond retention influencing documentation quality, care coordination, and clinical safety. As hospitals revisit their digital roadmaps, a shift toward inclusive, nurse-informed strategies could determine whether EHR systems evolve into a source of empowerment - or remain a factor driving nurses out of the profession.
About Black Book™
Black Book Research LLC is an independent, unbiased research organization specializing in healthcare technology and service user satisfaction. Its annual and quarterly surveys capture the voices of frontline clinical users, IT decision-makers, and administrators in more than 100 countries. Black Book has surveyed over half a million registered nurses and licensed nursing support professionals since 2010 and maintains a strict policy of no vendor sponsorship in their studies. Explore more insights and download free reports at: www.blackbookmarketresearch.com
Source: Black Book Research