New Stethoscope Design Hopes to Reduce Healthcare Infections
HOUSTON, April 23, 2020 (Newswire.com) - In a study by the Journal of Infection Prevention, “out of 62 participants, 53.22% had never cleaned their stethoscopes.” Initial swab samples showed over six types of bacteria growth. And that’s not counting viruses.
Furthermore, this is not just an American problem. A new stethoscope design is needed on a global scale. Canadian doctor Yves Longtin and Swiss doctor Didier Pittet wrote to the Mayo Clinic Proceedings urging that since doctors are not sanitizing their stethoscopes, “a more appealing, feasible, and scientifically sound solution is needed.” After seeing that “47% to 86% of health care workers do not disinfect their stethoscope regularly and only 6% to 15% disinfect their stethoscope after every use, […] clearly, future research is warranted to identify methods to decrease the infectious risks associated with the use of stethoscopes.” (All sources included in link.)
To put those percentages into perspective, in the most recent survey by the American Hospital Association, the U.S. alone has over 6,000 hospitals with over 900,000 staffed beds. In 2018 – a year without a severe illness outbreak – the U.S. saw over 36 million hospital admissions. Pair that with the WHO’s findings that “55 hospitals across 14 countries revealed an average of 8.7% hospitalized patients suffering from [healthcare-associated infections],” and it’s obvious that we can’t afford 3 million people to become infected through hospitals at any time, especially during a pandemic (Journal of Infection Prevention).
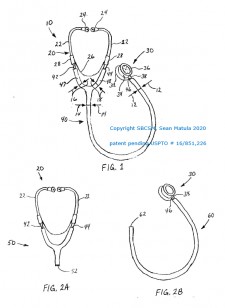
Universal Detachable Stethoscope Design
Engineering control solves the problem. This detachable stethoscope is broken into parts, just as with other medical equipment like thermometers and otoscopes. Instead of placing more strain and responsibility on healthcare workers to disinfect their stethoscopes throughout the day, this device decreases the risk of infectious disease transmission for both the healthcare provider and the patient.
One half of the device is assigned to the healthcare provider, and the other half of the unit is assigned to the patient. Designating separate parts greatly reduces the risk of disease transmission and protects both patients and workers in two ways:
- The upper half – earpieces and ear tubes – stay with the healthcare provider, reducing transmission from provider to provider.
- The lower half – acoustic tubing, bell, and diaphragm – are assigned to the patient, reducing risk of infection from patient to patient.
The design allows for conversion of all existing stethoscopes with an adapter kit. Assembly takes seconds, cutting the time it would take to fully sanitize an existing device.
Source: SBCSM